Osteochondrosis is a progressive degenerative change that affects the intervertebral discs. The pathology can appear in any part of the spine, but most often affects the cervical spine.
The problem cannot be neglected, as over time the symptoms increase and the pathology itself can result in serious health problems.

What is it
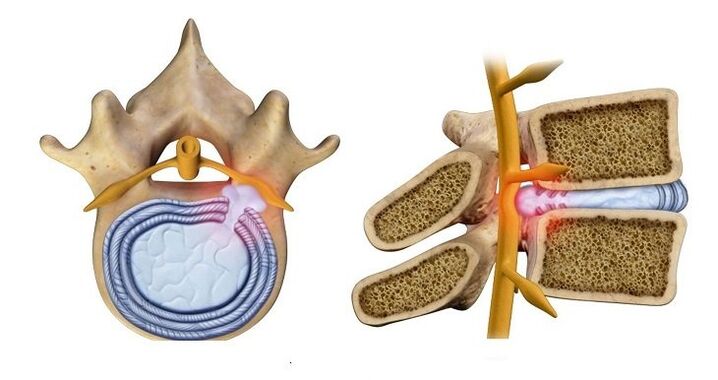
The human spine consists of individual vertebrae, between which there is a specific spacer - the intervertebral disc. It is formed by cartilaginous tissue and acts as a shock absorber, protects the bone tissue of the vertebra against abrasion and destruction, but at the same time flattens and wears it out.
Typically, these processes occur along with the aging of the human body and do not begin until the age of 50-55. But every year the pathology becomes younger, cases of premature wear of cartilaginous tissue have been recorded even in young people (25-30 years old).
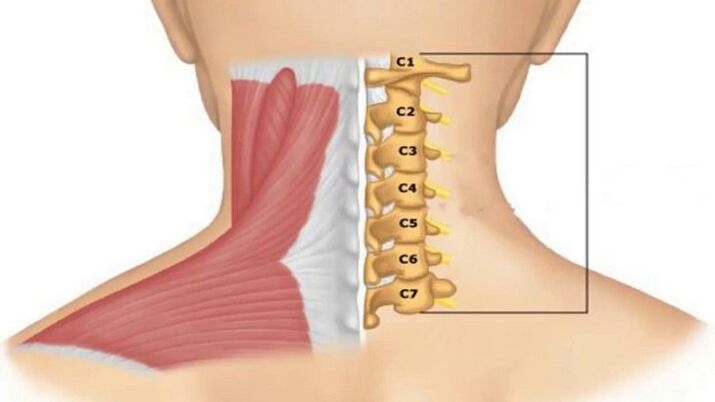
The high percentage of osteochondrosis of the cervical spine compared, for example, with the lumbar spine, is associated with loads on this specific part, caused by the need to keep the skull in a vertical position.
The weight of an adult's head can reach 3-5 kg: the weight of the skull bones is about 1. 400 g, approximately the same is the weight of the brain, about 500 g is the mass of blood circulating in the skull .
A feature of the cervical spine is the closer location of the vertebrae and the smaller thickness of the intervertebral discs, which leads to complications even with minor changes in them.
Reasons for development
Factors contributing to the development of pathological changes in cartilaginous tissue:
- sedentary lifestyle;
- forced tense postures during work (driving, at the computer);
- overweight;
- state of nervous tension;
- neck injuries;
- muscle weakness.
The neck muscles try to compensate for the load caused by these factors, resulting in spasms. Blood circulation, cartilage tissue nutrition and metabolic processes are disturbed, which leads to a change in its structure.
The following also play a role in premature aging of intervertebral discs:
- hereditary predisposition;
- autoimmune diseases that cause degeneration of cartilage tissue;
- congenital pathologies of spinal development.
Stages and symptoms of pathology development
Degenerative changes go through several stages, which are accompanied by specific symptoms:
Stage 1. The symptoms are still practically invisible. At this stage, it is possible to stop or slow down the pathological process without the help of medications (diet, exercise). The patient may feel:
- discomfort in the neck and shoulder muscles, tension, stiffness;
- mild pain when turning or tilting the head;
- headaches that occur infrequently and are of low intensity (more often appear after static or strenuous work, nervous experiences).
Stage 2. The height of the intervertebral discs decreases, compression of the nerve endings occurs, resulting in severe pain in the neck, especially when making movements and turns. Muscle spasm disrupts the blood supply to the skull, therefore, symptoms associated with vascular insufficiency are added. The person realizes:
- clicking in the neck joints when turning the head;
- decreased visual acuity;
- buzz;
- dizziness;
- frequent headaches for no apparent reason;
- numbness in the face and neck, loss of sensitivity in the skin of the hands and in the cervical collar region;
- sharp pains that radiate to the shoulder blade;
- sleep disorders.
Step 3. A herniated disc is formed (its nucleus protrudes into the spinal canal), which leads to disturbances in the functioning of the nervous system. Symptoms may include:
- numbness in the hands, paralysis of the upper limbs is possible;
- the pain affects the entire cervical collar region and can radiate to the heart region;
- "floaters" appear in the eyes, nausea and vomiting;
- feeling of a lump in the throat or pain, such as a sore throat;
- the skin on the upper part of the body may not even be felt;
- dizziness occurs with almost any movement;
- Headaches are migraine in nature.
Stage 4. Characterized by complete destruction of the disk:
- tinnitus may be permanent;
- dizziness may be accompanied by loss of consciousness;
- Coordination disorders appear as the blood supply to the cerebellar region of the brain is reduced.
Single intervertebral discs are affected extremely rarely. Generally the process involves the entire department. The destruction of individual disks can occur at different stages.
Diagnosis
Diagnosis of cervical osteochondrosis includes instrumental examinations and assessment of the symptom complex.
Of the instrumental methods, the main information will be provided by:
- x-ray - will show changes in the structure of the spine, but at advanced stages of the pathology;
- computed tomography - shows changes in the vertebrae, but it is difficult to distinguish between intervertebral hernias and compression of the spinal cord;
- MRI - allows you to see intervertebral hernias and the direction of their growth;
- Duplex ultrasound - shows the speed of blood flow in the area of suspected osteochondrosis.
When making the diagnosis, the doctor is based on the syndrome manifested in the patient. A syndrome is a combination of symptoms of a disorder.
With cervical osteochondrosis, the following syndromes may develop:
Vertebral- indicates that the pathological process involves bone and cartilaginous tissue. Manifestos:
- limited neck mobility;
- pain when turning the neck;
- structural changes in the vertebra or intervertebral disc (shown by x-ray).
Vertebral artery syndrome– means that the vertebral artery, which supplies blood to the brain, is involved in the pathological process. Main symptoms:
due to lack of blood flow:
- noise in the ears;
- dizziness;
- nausea and vomiting;
- pressure peaks;
due to irritation of the nerve endings of the artery:
- severe headache (migraine);
- numbness of the scalp skin;
- "floaters" in the eyes or temporary blindness;
due to lack of oxygen;
- fainting;
- lethargy;
- loss of ability to concentrate on anything;
- depression;
- panic attacks.
Cardiac.Signs similar to problems with the cardiovascular system:
- pain in the sternum (sometimes like a burning sensation);
- shortness of breath and fatigue;
- acceleration of heart rate.
Koreshkovy.Associated with impaired conduction of nerve impulses depending on damage to a specific pair of roots innervating the cervical region:
- 1st-2nd pairs of roots – pain or numbness in the back of the neck;
- 3rd pair – numbness of the tongue, difficulty chewing food;
- 4th pair – pain in the collarbone, lump in the throat, difficulty swallowing food;
- 5th pair – difficulty moving the arms with the problem concentrated in the shoulder region;
- 6th pair – discomfort in the shoulder blades and forearms;
- 7th pair – numbness in the hands, more often in the middle and index fingers;
- 8th pair – numbness of the ring and little fingers.
Treatment options
Only an integrated approach is applicable to the treatment of osteochondrosis. The fight against pathology can last many years.
Drug therapy
The use of medications for cervical osteochondrosis is aimed at:
- relieve pain;
- relieve inflammation and swelling;
- reduce muscle tension in the neck region;
- improve blood circulation;
- protect cartilaginous tissue from destruction and promote its restoration.
To diagnose and treat cervical osteochondrosis, you must contact a neurologist. If the clinic has a vertebrologist who directly treats spinal diseases, you can contact him immediately.
Your doctor may prescribe the following medications:
- Nonsteroidal anti-inflammatory drugs - relieve inflammation and swelling, reduce pain.
- B vitamins – help improve the functioning of nervous tissue.
- Chondroprotectors – protect cartilage tissue from destruction and restore its structure.
- Medicines that improve blood flow.
- Muscle relaxants are medicines that relieve muscle spasms.
Physiotherapeutic methods
Physiotherapy methods can quickly alleviate the patient's condition and are combined with medications:
- Electrophoresis– exposure of the affected area to low-intensity electrical current. Delivers medicinal substances directly to the problem area. It is usually prescribed with an anesthetic to relieve pain or with a medication to improve blood flow to the cervical region.
- Ultrasound– has anti-inflammatory properties, improves blood flow and metabolic processes.
- Magnetotherapy– helps to quickly relieve tissue swelling and improve metabolic processes.
- laser therapy– helps improve blood circulation at the site of exposure and also has an anti-inflammatory effect.

Massage
During drug and physiotherapeutic treatment, it is preferable to have a massage in the cervical collar region with a specialist.
Self-massage can be used in the future, only with great care, without trying to repeat the depth of impact demonstrated by a professional massage therapist.

When carrying out the procedure, the specialist uses classic massage techniques:
- stroking – activates the superficial layers of the skin;
- tighten – connects the deep layers of the skin;
- rubbing – warms the muscles and relaxes them, improves blood circulation;
- kneading - affects very deep tissues, so they are used with caution;
- vibration - knocks and shakes that end the procedure.
Manual therapy
Sometimes with cervical osteochondrosis it is recommended to consult a chiropractor. But this technique causes conflicting reviews: in some cases it certainly helps, in others it almost worsens the situation. The whole question is this:
- There is no doubt that a chiropractor must be a highly qualified doctor with medical training and qualifications as a neurologist or orthopedic traumatologist.
- Manual therapy for cervical osteochondrosis has many contraindications. Two people with similar symptoms may receive different answers about the need for manual therapy – one can and should, the other absolutely cannot.
To contact a chiropractor there must be strict instructions and no contraindications. They are determined by the attending physician and receive guidance for this type of therapy.
A highly qualified chiropractor will not work with a patient without studying the x-ray results.
Home treatment
Traditional treatment recipes or the use of any home remedies should be discussed in advance with the doctor, as in each specific case they can help or worsen the condition.
This applies, for example, to the needle applicator used. It consists of plastic spikes attached to a wide tape, which a person applies to the painful area (you can lie on them). The thorns cause irritation to skin receptors and increase local blood circulation. But it cannot be used for infectious and vascular diseases.
It is also common to warm the diseased area with mustard plaster or a bag of salt or sand. But with vascular diseases this can also be dangerous.
Therapeutic exercise (physiotherapy)
Therapeutic exercises are the safest method of treating cervical osteochondrosis. It is recommended to do this during an exacerbation and in the future - to prevent the disease.
The patient should not feel pain when performing the exercises. Doing this "in pain" will not only not bring any benefit, but can also harm your health.
The simplest but most effective movements are twists, bends and head rotations. It is strictly prohibited to do this at high speed and amplitude. Movements should be almost imperceptible. Despite low mobility, exercise ensures blood flow and improves circulation in the neck region.
Shants collar
The Shants collar is a rigid head support that relieves tension in the neck muscles and prevents movements that can cause pain. It is recommended to use both during treatment and for prevention of cervical osteochondrosis.
The collar is used constantly. The vertebrae are fixed in the correct position and do not exert pressure on each other, as well as on blood vessels and nerve endings. As a result, the pain disappears, blood circulation is normalized and many symptoms of pathology disappear.

If 5 to 7 cervical vertebrae are unstable, it will not be possible to use a bandage as it will not be possible to fix it in the correct position. It is also not recommended to use a collar if the thyroid gland is enlarged.
Orthopedic pillow application
Often, osteochondrosis is aggravated by compression of the cervical artery and nerve roots while sleeping on an uncomfortable pillow. An orthopedic pillow ensures a uniform horizontal position of the spine at night.
It alone does not cure osteochondrosis, but it alleviates the condition and is also a good measure to prevent the development of degenerative processes in the spine.
Prevention
There are simple rules that, if followed, will help prevent premature aging of intervertebral discs:
- monitor your weight: exceeding the norm by 10 kg creates a critical load on the entire spine;
- try not to lift or carry heavy things;
- if you need to carry a heavy bag, hold it alternately in your right and left hand (or it is better to use a backpack that evenly distributes the load across your entire back);
- every half hour of static work should be alternated with light exercise to relieve muscle tension and improve blood circulation;
- It is useful to practice physical education and sports exercises, for example swimming, but running, jumping and lifting weights are harmful to the spine;
- to sleep, use an orthopedic mattress and pillow.
Osteochondrosis of the cervical spine can significantly worsen a person's quality of life. The disease can be treated at an early stage, but as it develops, performing a daily series of exercises, following prevention rules, massages and other measures prescribed by your doctor will allow you to lead a comfortable life.






















